Finding Wholeness Through a Combination of Different Approaches: Q&A with Nekohl
Nekohl’s Story, May 2025
As told to: Diego Colón
Diagnosis received: Migraine, severe anxiety, post-traumatic stress disorder (PTSD)
Symptoms: Stress, dissociation, sensitivity to light, sensitivity to noise, head pain
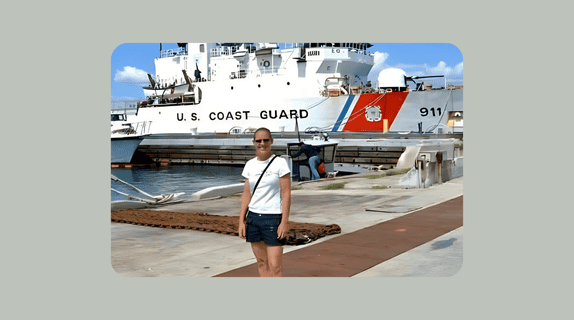
Nekohl, a former U.S. Army 92B-10 E-4 Medical Laboratory Specialist, served for eight years in a role that marked the beginning of a remarkable career in clinical laboratory leadership. Shortly after being deployed, she would begin experiencing symptoms that would take years to understand.
What initially seemed like stress-related headache attacks or a possible seizure-like disorder, her circumstances revealed a much more complex picture with one that included migraine, dissociation, severe anxiety, and post-traumatic stress disorder (PTSD).
Here, Nekohl reflects on her long journey towards receiving answers, the difficult decision of stepping back from a successful career and shares the importance of prioritizing one’s well-being to rebuild a life that is rooted in balance.
Q: Can you tell us about your military background?
I left the military after eight years… I was a specialist, 92B-10 [E-4] Army Medical Laboratory Specialist.
Q: How did your headache or migraine journey begin?
My diagnosis was not a diagnosis for a couple of decades. [I] started up in the military. I went through basic training, AIT [Advanced Individual Training]. For a short period of time, I was doing my military duty, and very shortly after, I got called over to the Persian Gulf… I hadn’t suffered [from] headaches at all my entire life. I didn’t have to take aspirin or anything for headaches.
[When visiting a healthcare provider,] they tried to travel back to figure out where my problems started… I got married when I was 22, [and] I started having obvious symptoms. Maybe [by] 2021, [was] when I would have a headache here and there, but nothing that I could pin on saying I [definitely] had migraines. My migraines came a little differently, [and] the doctors were confused. They thought I had some seizure-like disorder… or that it was connected with dissociation, but [to clarify,] I didn’t have a whole lot of bad headaches.
Q: As you climbed up the ladder, how did your symptoms start to show up or change?
… I would have headaches when I was stressed out. I was working in management and… I did have some presentations of migraines, but bigger than that [was] the anxiety, dissociation, coupled with headaches.
If I had headaches [for] too long, I would have an anxiety attack… I was losing time at my desk, disconnecting, and they couldn’t figure out what it was, so they said, ‘Maybe you have some kind of seizure-like disorder.’

I started my career in the laboratory for the military. I went up through the ranks. I went from phlebotomist to lab tech supervisor, manager, and director of lab and cardiopulmonary services and… corporate compliance
I just went up, up, up, and up, which really looks good, but the closer I got to the top, the worse my symptoms became.
Q: Have your symptoms ever affected your ability to perform your tasks while at work?
I remember [a specific attack happening] in 2014 like [it was] yesterday. [I was] having a headache so bad that I couldn’t even stand for the phone to ding. By being [in] management, I got phone calls and pages… all day and night. I was on call 24/7. It got so bad that I couldn’t stand to hear the ding from the phone, so I would have to turn it down. I was missing emergent circumstances because when my phone would ding ding ding, it bothered me, so I turned it off. I couldn’t do anything about it, which is when I started applying for FMLA [Family Medical Leave Act] so that I wouldn’t lose my job.
I would take time off when I got those headaches… I’ll have to take a day off because I couldn’t even stand for the phone to ding... When you’re on call 24/7, you got to get somebody else to be on call for you, because if I don’t hear the phone, I can’t handle anything that’s happening in the laboratory.
I remember my worst migraine before I started getting treatment was that something emergent had happened in the lab. I had to tell my boss… ‘I can’t stand for the phone to ring, so I won’t be able to be on call, I can’t be available.’ She wasn’t happy about it…But I was protected on family leave because it went by the year. [However], it went up, up, up, the amount of time I had to take off increased… until the point that I had to start going down in my position…
…I got up to [be] Assistant Director of Clinical Support Services at UIC. Big job. Great job, [but it was] too much for me. I remember being there one time, and I had to get on the floor because my head was hurting so bad. I don’t know if I passed out or dissociated… it was really bad… I scared the life out of my staff because they didn’t know what to do… I started to go down in my profession [after that incident]…
Q: In light of these workplace challenges, how did you begin to prioritize your health?
I had to make a decision to do something different. For a year, I did nothing at all because I was getting treated for all that was going on. It had gotten to the point where I was dissociating really bad, and I had to be treated with medication for that. I did go through day hospital, which was a program to try to figure out what exactly was going on with me. So, it ended up being a combination of things: migraines, dissociation, severe anxiety, and PTSD.
[Through the military], I went through a day hospital program where I go in every day and get the treatment that I needed for my psychological health. A lot of the medications they gave me were something that worked for migraines and anxiety. If I have a migraine [for] too long, I’ll have anxiety attacks, and vice versa. My anxiety attacks caused me to have a headache when I came down from it, so they gave me medication, and the military was really good to me. I went through day hospital for five weeks… [and] did an emergency program for two weeks.
It’s impossible in my case for my migraines to become better. My psychological health is not helped [or being managed effectively]. It’s not well because they work on each other. Once I get overwhelmed, I’m going to have a horrible headache, [and] once I come down from dissociating or having [an] anxiety [attack], I have a headache. So they need to get me something that’s going to work for all of those [symptoms].
Q: What does your current approach to managing your symptoms look like, and has it been effective?
Sometimes I get tired of taking medication, and I stop, like most people do, like ‘Okay, I think I’m good,’ [but] that’s when the headaches will come or I might have a little dissociating. It’s a combination of experiences that I don’t like, nor do I like that this is part of my diagnosis, and I have to deal with it

But I don’t only use medication. I meditate. I use [a] whole lot of different wholeness practices to keep myself grounded. [I turn to migraine hacks, using] a lot of ice water, some cold baths, [and] walking. There are a lot of things that I do as a combination to keep me whole… I don’t take as much medication as I once did…
But now I have a pretty good regimen, and I can scale it up if I need to or scale it down. My doctor and I have a really good relationship [as well as with] my medication!
The three of us work together very well, along with the different tools that I use, [which] I created a custom way to use these tools… now I meditate, or I’ll take a walk… It’s a lot of different things that, as a combination, work together for me to maintain wholeness
Q: What advice or guidance would you give yourself if you could speak to the version of you who had their first migraine attack?
Choose yourself. Back then, when I felt myself changing and experiencing things that I had never experienced before, I continued to try to go on with life as usual, [by] taking care of the job, working 8-12 hours a day [and] trying to make sure those surveys are passed, and the staff is OK, that my family is OK, and that everything else around me was balanced…
I would tell her, ‘Girl, if you need to take [time] off, take off. If you don’t feel good, stay home. Find out what’s going on so that you can become a better version of yourself now instead of waiting two decades from now.’ Do it now. Take care of you. Get all the information, education, and resources that you need so that you can evolve gracefully. Find out what tools you need so that you can create balance every day. Become whole every day…
Q: What guidance would you share with other veterans who might be navigating similar experiences to yours?
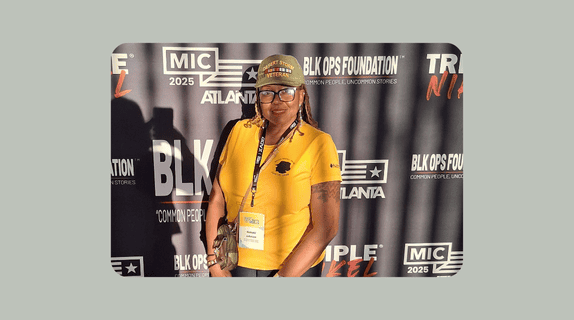
… Don’t be afraid of trying something different. When I had to change my entire life for my health, the change was very challenging. I had to become worse before I could become better. I had to break down the old version of myself and build up a new person who I don’t fully even know yet… We continue to evolve, so allow yourself to evolve into a different space… walk carefully into that space and provide yourself with everything you need to be content day by day.
… That’s my purpose in life to help one person, and I know that one person can reach thousands [of people]… Don’t try to do it all at one time… [I] make sure that for today I have what I need to be whole, healthy, and content. Even if it’s not all happy days, because it won’t [always] be easy… [know] you can make it through
Learn more about dissociation and PTSD: